Easy extras claiming options
There are several options for making a claim on your extras membership.
- Claim without your physical card, using the QR Code in your app - simply open your app on your smartphone, click Create HICAPS QR code and scan at any HICAPS Trinity machine.
- Claim on the go with the Latrobe Health app from your mobile phone or tablet – simply snap a picture of your receipt and we will put the money into your account.
- Claim on this site using our online claim form.
- Claim on the spot - swipe your membership card at the time of receiving your treatment with registered providers.
- Submit a claim form by post or visit one of our branches - the payment will be put into your bank account.
Need more information? See below.
Claim using the app
Search for Latrobe Health Services in the Apple Store (iOS) or Google Play Store (Android) and start claiming on the go using the QR Code or upload receipts, track claims, check your benefits and limits, see your payment details, update your contact info and find a provider near you.
iOS |
Android |
 |
 |
 |
 |
Claiming made easy with Latrobe Health’s new cardless option
We’re excited to introduce QR Code claiming via the Latrobe Health app, making it easier than ever to claim on-the-spot at participating providers using a secure QR code.
How it works
With HICAPS (Health Industry Claims and Payments Service) Australia’s leading electronic claiming system you can now scan your digital QR code at providers with HICAPS Trinity terminals and have your claim processed instantly. The QR code will on work on HICAPS Trinity machines, not Tyro or Healthpoint.
Getting started is simple
1. Download or update the Latrobe Health app
- New to the app? Download it from the App Store or Google Play and register for online access.
- Already using it? Make sure your app is updated to the latest version to unlock digital claiming.
2. Create your QR code one of two ways;
- Open the app and tap ‘Create HICAPS QR code’, or
- Tap the ‘Profile’ icon and select ‘Create HICAPS QR code’. Your QR code refreshes regularly for added security (so please don’t screenshot it or print it out).
3. Claim on the spot
- Scan your QR code at the provider’s terminal until you hear a beep.
- The provider will confirm if your claim is approved. If there’s a gap or your benefit limit has been reached, you’ll only need to pay the difference.
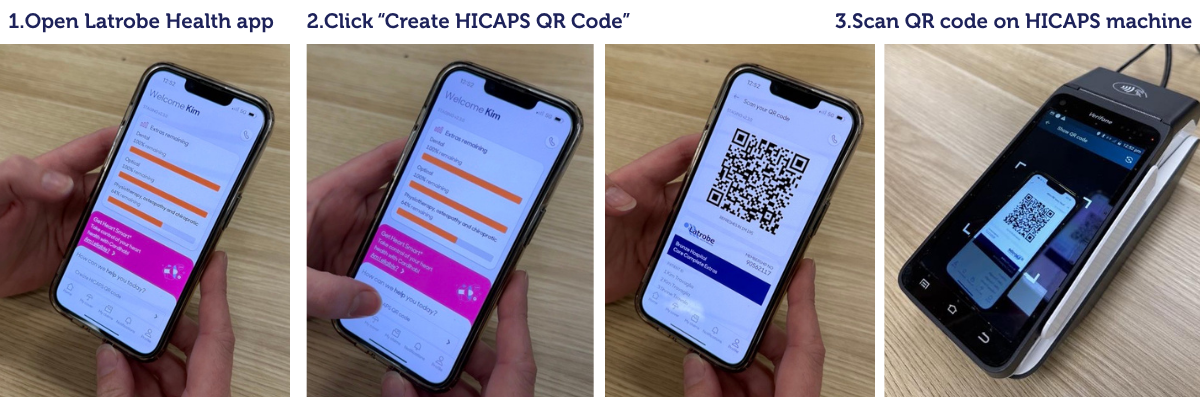
Claiming for someone else on your policy? Just let the provider know who the claim is for and their position number shown on the QR code screen.
Note: Some services aren’t eligible for on-the-spot claiming, such as those requiring extra documentation (e.g. health management programs, most aids and appliances, orthodontics).
Find out more in the FAQ below.
Claim on the spot
The following services are claimable via HICAPS or HealthPoint with participating providers. Check with your provider and present your card to claim your benefit immediately.
- Chiropractic
- Dental
- Dietetics
- Osteopathy
- Physiotherapy
- Podiatry
- Speech therapy
- Optical
- Psychology
- Chinese medicine
- Exercise Physiology
- Acupuncture
- Massage
- Myotherapy
You may find the following services are not often claimable through HICAPS or HealthPoint, and therefore we recommend either using the mobile app, or completing a claim form and either posting it to us, visiting us in branch, or emailing your completed claim form.
- Audiology
- Eye therapy
- Heath screenings
- Prosthesis
- Mouth guards
- Orthotics
- Pharmacy
- Occupational therapy
- Lymphoedema garments
- Home services/visiting nurse
- Preventive/health management appliances
Claim online
Claiming on our website is quick and easy. Simply complete the form and upload your receipt. Your claim will be assessed by our team and once approved your benefit will be paid into your nominated bank account in three to five days.
Claim directly with Latrobe Health
You can make a claim at any Latrobe branch or by mailing all the necessary documentation to us.
- A claim form should be completed in full, including your current address and contact details.
- Sign the claim form and post with your original receipt to Reply Paid 41, Morwell VIC 3840.
- Benefits are paid directly into your account.
What details do I require from the provider?
All accounts must show:
- Date(s) of service
- Type of service
- Patient name
- Provider name and address on official letterhead
- Provider number
If your provider does not supply you with an account with all of the above details a benefit cannot be paid.
How long do I have to make a claim?
If claims are not made within two years of the date of service, benefits are not payable. We recommend that you submit all claims as soon as practicable after the service is provided.
How to make a claim on the mobile app
Everything you need to know about making a claim on your mobile app
